Now more than ever we are aware of the impact of post-traumatic stress disorder (PTSD) on veterans returning from the front lines of wars in the middle east, raging for the last ten years. These wounded warriors often respond poorly to traditional treatment with drugs aimed at adjusting levels of brain neurotransmitters which in part mediate the abnormal response to stress. PTSD is characterized by repeated re-experience of traumatic events, avoidance symptoms, including reluctance to think or talk about the trauma, and excessive arousal symptoms, including poor sleep and poor concentration.
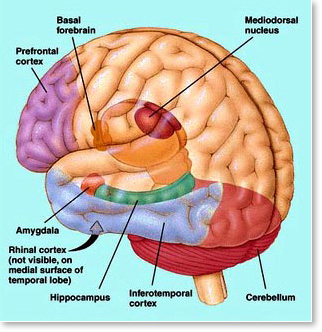
What is the biologic basis of this disorder? Though all of the puzzle pieces have not yet been put together, we do know that certain parts of the brain responsible for explicit memory (ie. the verbal memory of the event) and emotional reaction do not function normally in people afflicted with PTSD.
1. The gateway of memory, the hippocampus, located near the undersurface of the brain, is reduced in size in many PTSD patients, apparently because of the negative effect of stress hormones on the nerve cells that make up this structure. The result is memory impairment and amnesia for some events.
2. A neighboring structure, the amygdala, is abnormally activated in PTSD. The amygdala infuses memories with strong emotion, and its excessive activity can trigger anger and rage reactions.
3. The prefrontal cortex, the seat of judgment and planning, thought to act as a counterbalance to the impulsive amygdala, is also negatively affected in PTSD.
PTSD has traditionally been treated like other anxiety disorders characterized by episodic flare-ups, which are incapacitating. Drugs aimed at treating both anxiety and depression are utilized, as are behavioral therapies, all with limited success.
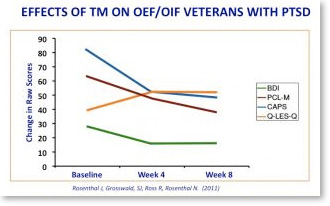
By the fourth week of practicing TM, OEF/OIF veterans with PTSD experienced dramatic reductions in PTSD symptoms according to the Clinically-Administered PTSD Scale (the gold standard of PTSD testing). They also reported decreased depression and improved quality of life—showing a greater ability to return to their lives after the war. These findings replicated an earlier study examining TM as a treatment for Vietnam veterans with PTSD.
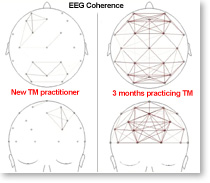
The recent pilot study showing a 50% reduction in PTSD symptoms in veterans practicing Transcendental Meditation is welcome news, and not unexpected. After all, it fits with what we know about TM and how it affects the brain. During TM, the EEG changes reflect prefrontal cortical activity naturally and effortlessly increasing in power in a coherent manner.
The state of restful alertness during TM is exactly the opposite of what we see with amygdala over-activity. And, we see these EEG changes during TM even in new meditators, so a few weeks or months of practice can be expected to significantly reduce the negative impact of repeated episodes of emotion-laden memories. The memories are not erased, but they are less likely to overwhelm, as this new style of a more coherent cortical functioning is established in the brain of someone practicing TM twice a day.
 What a great addition this is to the arsenal of physicians treating these wounded warriors, and also non-veterans who have been affected by PTSD and anxiety disorders. We must all work to make it available to those in need.
What a great addition this is to the arsenal of physicians treating these wounded warriors, and also non-veterans who have been affected by PTSD and anxiety disorders. We must all work to make it available to those in need.
References:
Neurobiology of Posttraumatic Stress Disorder; D. Jeffrey Newport and Charles B. Nemeroff; Focus 1:313-321 (2003) Am. Psychiatric Assoc.
Effects of Transcendental Meditation in Veterans of Operation Enduring Freedom and Operation Iraqi Freedom With Posttraumatic Stress Disorder: A Pilot Study; Rosenthal, Joshua Z.; Grosswald, Sarina; Ross, Richard; Rosenthal, Norman; Military Medicine 176: 6 pp. 626-630 (2011)
——————————————
![]() Dr. Gary Kaplan is a neurologist and Associate Professor of Clinical Neurology at Hofstra University School of Medicine. Dr. Kaplan received the Albert H. Douglas Award from the Medical Society of the State of New York for outstanding achievements as a clinical teacher interested in promoting and improving the medical education of physicians. He is also a nationally recognized expert on the effects of the Transcendental Meditation program on stress-related illnesses, and he appears regularly on CNN, NBC and CNBC and other national television programs speaking about the latest research on Transcendental Meditation and its effects on health.
Dr. Gary Kaplan is a neurologist and Associate Professor of Clinical Neurology at Hofstra University School of Medicine. Dr. Kaplan received the Albert H. Douglas Award from the Medical Society of the State of New York for outstanding achievements as a clinical teacher interested in promoting and improving the medical education of physicians. He is also a nationally recognized expert on the effects of the Transcendental Meditation program on stress-related illnesses, and he appears regularly on CNN, NBC and CNBC and other national television programs speaking about the latest research on Transcendental Meditation and its effects on health.